We have composed a few answers to common questions from patients about common shoulder and elbow conditions. We hope you find some useful information.
ROTATOR CUFF TEAR
What is the Rotator Cuff?
The Rotator Cuff is a group of 4 muscles and tendons (supraspinatus, infraspinatus, subscapularis and teres minor) responsible for the stability and movement of the shoulder. Apart from its role as a rotator of the shoulder, the integrity and contraction of the rotator cuff muscles keeps the ball of the joint centered on the socket.
What are Rotator Cuff Tears?
They are disruptions in the continuity of any of the 4 rotator cuff tendons which maybe traumatic (as a result of an injury) or degenerative (age-related). Rotator cuff tears are rare in patients under the age of 40.
The supraspinatus is the most commonly torn tendon and the symptoms felt by patients vary from severe pain and functional disability to no symptoms whatsoever. Partial tears may heal naturally but full thickness tears do not, however many patients learn to compensate with other muscles to function normally. We do not yet understand why some patients experience problems and some do not.
What are the symptoms of Rotator Cuff Tears?
The most common symptom is pain and weakness when lifting the arm overhead. Typically the pain is better with rest and worse with movement. For large tears patients may not be able to lift the arm at all without help.
What is the treatment for Rotator Cuff Tears?
Pain relief and a good level of functional recovery can be achieved with painkillers and physiotherapy for patients with rotator cuff tears. However for those with on-going problems, a recent large UK study (The UKUFF Trial) has shown that rotator cuff repair surgery is effective in reducing pain and improving function.
Some tears can progress (become larger) over time and can be accompanied by arthritis in the shoulder over a number of years if not repaired.
What type of surgery is involved?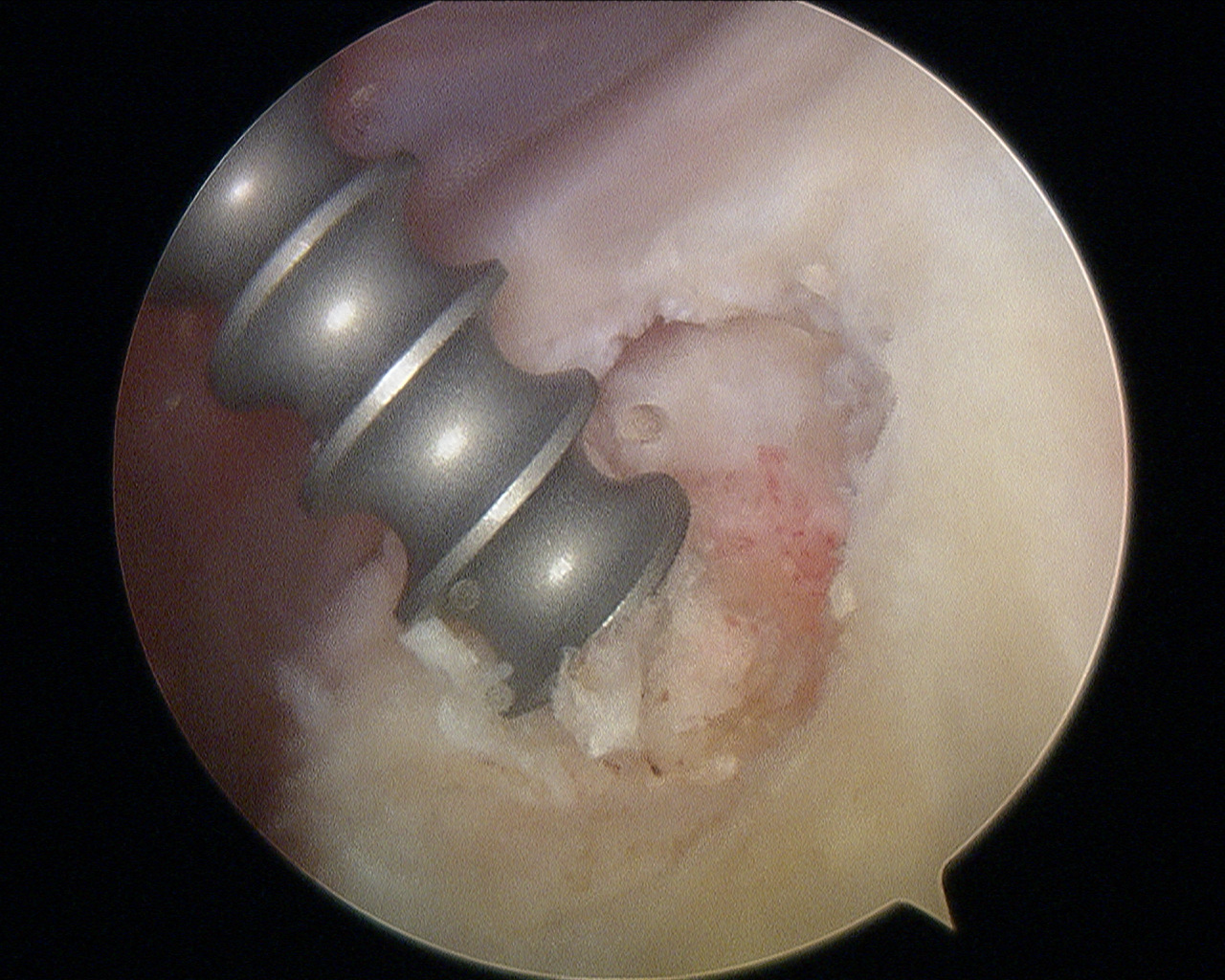
There are a number of ways to treat rotator cuff tears. These include Open, Mini-open and Arthroscopic (keyhole) techniques. Open is the classical technique; Arthroscopic is the “keyhole” approach while mini-open is the intermediate (small open) approach.
Arthroscopic rotator cuff repair is preferred over the older techniques because it allows the surgeon to treat all coexisting pathologies with the same small incisions whilst providing a more rapid recovery.
Surgery to repair a torn rotator cuff most often involves re-attaching the tendon to the bone, however if there are additional problems such as arthritis or the tear is too large to repair alternative surgical options may be required. We will discuss with you the best procedure to meet your individual health needs.
FROZEN SHOULDER
The medical name is Adhesive Capsulitis. It affects the ligament capsule of the shoulder joint which becomes inflamed and over time thickens with scar tissue causing restriction of movement. Nobody knows why it starts. It can be triggered by a minor injury or shoulder surgery but usually occurs for no reason. We know that it usually affects adults aged 40-65 and is more common in people with diabetes or thyroid disorders.
What are the symptoms?
The typical features are of pain in the upper arm (rather than just the shoulder itself) that is bad enough to disturb sleep. There is pain even at rest. Fast movements of the shoulder can cause severe pain. Initially shoulder range of movement may not be affected but as time passes the shoulder becomes increasingly stiff. Rotational movements are worst affected such as reaching behind your back or behind your head.
What is the treatment for Frozen Shoulder?
A Frozen Shoulder will improve naturally over time but this can take up to two years, or longer in extreme cases. Steroid injections combined with stretching exercises are effective in reducing pain and improving function for the majority of patients.
When conservative treatments do not help, the options include a manipulation of the joint shoulder whilst the arm is anaesthetised or keyhole surgery (called arthroscopic capsular release). Both of these procedures are done as day surgery without the need for an overnight stay.
SHOULDER ARTHRITIS
Osteoarthritis also known as “wear-and-tear” arthritis is a condition that erodes the smooth lining (articular cartilage) of a joint. As the cartilage wears away, it becomes frayed and rough, and the protective space between the bones decreases. During movement, the bones of the joint rub against each other, causing pain.
Osteoarthritis usually affects people over 50 years of age and is more common in the acromioclavicular (end of collar bone) joint than in the glenohumeral (ball and socket) shoulder joint.
There are other forms of arthritis that can affect the shoulder joint including rheumatoid arthritis. Rheumatoid arthritis is an inflammatory process that affects the lining of the joint causing swelling and pain.
Post-traumatic arthritis can occur after fractures of the upper arm bone or dislocation of the shoulder joint.
Rotator cuff tear arthritis occurs after large, longstanding rotator cuff tendon tears. The torn rotator cuff can no longer hold the ball of the joint firmly in the socket, causing it to rub up and down. This can damage the surfaces of the joint, causing arthritis to develop.
What are the symptoms of shoulder arthritis?
The most common symptom of arthritis of the shoulder is pain, which is aggravated by activity and progressively worsens.
If the glenohumeral (ball & socket) shoulder joint is affected, the pain can be felt all around the shoulder spreading into the upper arm. The pain is often worse and the shoulder more stiff to move first thing in the morning.
The pain of arthritis in the acromioclavicular (AC) joint is focused on the top of the shoulder at the end of the collarbone. This pain can sometimes radiate or travel to the side of the neck.
Someone with rheumatoid arthritis may have pain throughout the shoulder if both the glenohumeral and AC joints are affected.
Limited motion is another common symptom. It may become more difficult to lift your arm to comb your hair or reach up to a shelf. You may hear a grinding sound (crepitus) as you move your shoulder.
As the disease progresses, any movement of the shoulder causes pain. Night pain is common and sleeping may be difficult.
What are the treatment options for shoulder arthritis?
As with other arthritic conditions, initial treatment of arthritis of the shoulder is nonsurgical. This includes activity modification to avoid provoking pain. Anti-inflammatory medication including oral painkillers and corticosteroid injection in the shoulder can reduce the inflammation and pain.
Surgical treatment is reserved for patients with failed nonsurgical treatments.
Is there a “keyhole” procedure to treat shoulder arthritis?
In cases of mild glenohumeral arthritis it could be treated with arthroscopy (“keyhole”) surgery. During arthroscopy, the surgeon inserts a small camera, called an arthroscope, into the shoulder joint. The camera displays pictures on a television screen, and the surgeon uses these images to guide miniature surgical instruments.
Because the arthroscope and surgical instruments are thin, the surgeon can use very small incisions (cuts), rather than the larger incision needed for standard, open surgery.
During the procedure, the surgeon can debride (clean out) the inside of the joint. Although the procedure provides pain relief, it will not eliminate the arthritis from the joint. If the arthritis progresses, further surgery may be needed in the future.
Arthritis of the acromioclavicular joint is commonly treated by removing a small amount of bone from the end of your collarbone, leaving a space that gradually fills with scar tissue making a false joint. This can be done to through a keyhole or an open technique.
In moderate to severe glenohumeral arthritis patients may need other surgical treatments such as a shoulder replacement.
What is a shoulder replacement?
Advanced arthritis of the glenohumeral joint can be treated with shoulder replacement surgery, in which the damaged parts of the shoulder are removed and replaced with artificial components made from metal and plastic.
Replacement surgery options include:
Hemiarthroplasty. Just the ball of the joint is replaced by an artificial component.
Total shoulder arthroplasty. Both the ball and the socket are replaced. A plastic “cup” is fitted into the socket, and a metal “ball” is attached to the top of the arm.
Reverse total shoulder arthroplasty. In a reverse total shoulder replacement, the socket and metal ball are the opposite way around compared to a conventional total shoulder arthroplasty. The metal ball is fixed to the socket and the plastic cup is fixed to the upper end of the arm. A reverse total shoulder replacement is designed for patients with torn rotator cuff tendons to allow them to use other muscles to raise their arm.
What is the recovery after shoulder replacement surgery?
Surgical treatment of arthritis of the shoulder is generally very effective in reducing pain and restoring motion. Recovery time depends upon the type of surgery performed, but typically patients need to wear a sling for four weeks and it often takes at least three months to settle fully.
What are the complications of shoulder replacement surgery?
As with all surgeries, there are some risks and possible complications. Potential problems after shoulder surgery include infection, excessive bleeding, blood clots, and damage to blood vessels or nerves. Particularly with shoulder replacement surgery the artificial joint may wear and loosen over time, which may require further surgery in the future.
We will discuss the possible complications with you before your operation.
Download our Total Shoulder Replacement Information Booklet here.
SHOULDER INSTABILITY
What is shoulder instability?
The shoulder is the most flexible joint in your body. It helps you to lift your arm, to rotate it, and to reach up over your head. It is able to turn in many directions. With this greater range of motion, however, it can be vulnerable to instability.
Shoulder instability occurs when the ball of the joint is forced out of the shoulder socket. This usually happens as a result of a sudden injury but can happen without an injury if a person is unusually flexible.
Shoulder dislocations can be partial, with the ball of the upper arm coming just partially out of the socket. This is called a subluxation. A complete dislocation means the ball comes all the way out of the socket.
Once a shoulder has dislocated, it is vulnerable to repeat episodes. When the shoulder is loose and slips out of place repeatedly, it is called chronic or recurrent shoulder instability.
What are the symptoms of shoulder instability?
Common symptoms of chronic shoulder instability include:
- Pain caused by shoulder injury
- Repeated shoulder dislocations
- Repeated instances of the shoulder giving way
- A persistent sensation of the shoulder feeling loose, slipping in and out of the joint.
What are the treatment options for shoulder instability?
Chronic shoulder instability is often first treated with nonsurgical options. If these options do not relieve the pain and instability, surgery may be needed.
Nonsurgical Treatment
It often takes several months of nonsurgical treatment before you can tell how well it is working. Nonsurgical treatment typically includes:
Activity modification: You must make some changes in your lifestyle and avoid activities that aggravate your symptoms.
Physiotherapy: Strengthening shoulder muscles and working on shoulder control can increase stability. Your physiotherapist will design an exercise program for your shoulder.
Surgical Treatment
Surgery is often necessary to repair torn or stretched ligaments so that they are better able to hold the shoulder joint in place.
Arthroscopy (keyhole surgery). Soft tissues in the shoulder can be repaired using tiny instruments through small incisions. This is usually a same-day procedure. Arthroscopy is a minimally invasive surgery. We will look inside the shoulder with a tiny camera and perform the surgery with special small instruments.
Open Surgery: Some patients may need an open surgical procedure. This involves making a larger incision over the shoulder and performing the repair under direct visualisation.
In more severe cases where there is significant bone loss in the ball and socket joint a bone graft procedure may need to be performed known as a Latarjet procedure.
Will I need physiotherapy after surgery?
Yes. After surgery, your shoulder may be immobilised temporarily with a sling.
When the sling is removed, exercises to rehabilitate the shoulder will be started. These will improve the range of motion in your shoulder and prevent scarring as the ligaments heal. Exercises to strengthen your shoulder will gradually be added to your physiotherapy plan.
It is important to follow the postoperative rehabilitation plan. Although it is a slow process, your commitment to physiotherapy is the most important factor in returning to normal activities after surgery.
CALCIFIC TENDINITIS
What is Calcific Tendinitis?
 This is a condition where calcium forms within the tendons of the rotator cuff. Sometimes this is painless and is only diagnosed when patients have an x-ray for another reason. Sometimes, however, it can cause inflammaton of the surrounding tendon resulting in significant pain.
This is a condition where calcium forms within the tendons of the rotator cuff. Sometimes this is painless and is only diagnosed when patients have an x-ray for another reason. Sometimes, however, it can cause inflammaton of the surrounding tendon resulting in significant pain.
What are the symptoms?
When symptomatic, calcific tendinitis is extremely painful. It can start without reason but usually is caused by a trivial injury. Patients usually complain of a throbbing pain at rest that becomes severe with movement of the elbow away from the body.
How is it diagnosed?
Calcium deposits can usually be seen on a simple x-ray. Very small deposits may be overlooked but can be seen on ultrasound scan.
What are the treatments?
The calcium eventually will be reabsorbed by the body so one option is to use painkiller or anti-inflammatory medication and wait. If the pain is still poorly controlled then steroid injections can be effective. In extreme cases keyhole surgery can be performed where the surgeon makes a small cut in the surface of the tendon and squeezes the calcium out like toothpaste.
TENNIS ELBOW
What is Tennis Elbow?
It is pain arising from the tendons on the outside of your elbow. It tends to occur following repetitive gripping or activities that involve the wrist extending backwards (similar to playing a game of tennis). It usually affects people of middle age. The exact cause is however not clearly understood.
What are the symptoms?
Pain on the outside of the elbow is the most common presentation. The pain exacerbates on lifting heavy objects, on making a fist, or on repetitive activities such as typing. Swelling is not common. The elbow is tender on pressing the bony lump present on the outside (lateral epicondyle).
How can you treat this condition?
The treatment depends on the severity of the condition. Activity modification i.e reducing repetitive activities that excite pain should be undertaken initially. Anti-inflammatory medications can help relieve the pain in the short term. Some people find Tennis Elbow Clasp splints helpful.
The most effective conservative treatment is specific Physiotherapy strengthening exercises. This can be organised by your GP. Steroid injections help the pain in the short term but have been shown to increase the risk of the symptoms returning and may delay healing in the long term.
A specialist input should be obtained if the pain is not relieved despite at these measures as further treatment may involve use of PRP (Platelet Rich Plasma) injections and open surgery.
How long is the recovery following surgery?
A full recovery following surgical intervention may take 3-6 months
GOLFER'S ELBOW
What is Golfer’s Elbow ?
It is pain arising from the tendons on the inside of your elbow. It tends to occur following repetitive gripping or activities that involve the wrist flexing forwards (similar to playing a game of golf). It usually affects people of middle age. The process is similar to tennis elbow and the cause is not fully understood.
What are the symptoms?
Pain on the inside of the elbow is the most common presentation. The pain exacerbates on firm grasps with wrist bending. The elbow is tender on pressing the bony lump present on the inside (Medial epicondyle).
How can you treat this condition?
The treatment depends on the severity of the condition. Activity modification i.e reducing repetitive activities that excite pain should be undertaken initially. Anti-inflammatory medications can help relieve the pain in the short term. Some people find Golfer’s Elbow Clasp splints helpful.
The most effective conservative treatment is specific Physiotherapy strengthening exercises. This can be organised by your GP. Steroid injections help the pain in the short term but have been shown to increase the risk of the symptoms returning and may delay healing in the long term.
A specialist input should be obtained if the pain is not relieved despite at these measures as further treatment may involve use of PRP (Platelet Rich Plasma) injections and open surgery.
How long is the recovery following surgery?
A full recovery following surgical intervention may take 3-6 months
ELBOW ARTHRITIS
What is Elbow Arthritis?
The most common type of arthritis is Osteoarthritis. The is wearing of the smooth cartilage surface of the elbow joint due to aging. Arthritis can also be caused from a previous fracture or by the less common Rheumatoid Arthritis.
What are the symptoms?
Onset of symptoms is typically seen in patients older than 50years of age, but some patients can have symptoms earlier. The commonest symptom is pain, often described as a dull ache. This can also be associated with stiffness, usually worst in the morning, and restricted elbow range of movement. You may feel ‘grating’ in the elbow joint due to the wear or ‘locking’ if there are loose bits of cartilage inside the joint.
How can it be diagnosed?
The diagnosis of the condition is based on the history of symptoms, clinical examination of the joint and an x-ray of the elbow joint.
How can it be treated?
Treatment is based on the clinical presentation, X-ray findings, stage of the arthritis and patient’s expectation. Initial management includes pain killers and anti-inflammatories. Physiotherapy and activity modification is advised as this helps in pain alleviation with maintenance of elbow movement. Corticosteroid injections are sometimes used if the pain is not well controlled with painkillers.
Surgical treatment is advocated when nonsurgical interventions are not enough to control symptoms. For mild to moderate arthritis, a debridement (cleaning out) procedure can help with pain and may increase range of elbow movement. In severe cases, a total joint replacement may be advised.
CUBITAL TUNNEL SYNDROME
What is cubital tunnel syndrome?
It is a compression or irritation of the nerve (ulnar nerve) as it runs down the inside of the elbow. The nerve lies in a small groove in the bone of your elbow. In some patients, the nerve slips in and out of the groove as the elbow is bent and straightened. If this occurs repetitively, the nerve may be significantly irritated. In some cases the nerve can be compressed by a slow build-up of scar tissue.
What are the symptoms of Cubital tunnel syndrome?
The commonly described symptoms are-
- Pins and needles – This is typically the first symptom and usually affects the ring and little fingers.
- Pain in the same fingers may then develop. Pain is also experienced around the forearm or elbow.
- Numbness may develop if the condition becomes worse.
- Weakness resulting in poor grip and clumsiness
- Muscle wasting between the fingers.
The symptoms are usually felt when there is pressure on the nerve, such as sitting with the elbow on an arm rest, or with repetitive elbow bending and straightening.
Do I need any tests?
If symptoms are persistent, nerve conduction tests can be arranged to measure the severity of nerve compression. Ultrasound scans can be used to investigate whether the nerve is slipping out of the groove.
What is the Treatment?
Use painkillers to ease the pain, keeping the elbow straight at night with a splint also may help. If symptoms continue to be intrusive surgical opinion should be obtained. Decompression of a compressed nerve prevents symptoms from getting worse and often can restore normal sensation. A slipping nerve can be moved to prevent irritation.
CARPAL TUNNEL SYNDROME
What is the Carpal Tunnel Syndrome?
It is compression of one of the nerves to the hand (Median Nerve) as it travels through the carpal tunnel of the wrist. It is often associated with occupations involving heavy labour. It is also relatively common during pregnancy but the symptoms usually settle after childbirth.
What are the symptoms of carpal tunnel syndrome?
The symptoms vary according to the severity of the condition. They are generally worse at night and may wake you up. The symptoms can be eased by moving the wrist and fingers.
The commonly described symptoms are-
• Pins and needles – This is typically the first symptom and usually affects the thumb, index and middle fingers.
• Pain in the same fingers may then develop. The pain may travel up the forearm.
• Weakness resulting in poor grip and eventually leading to muscle wasting at the base of the thumb can also be seen.
Do I need any tests?
When symptoms persist, nerve conduction tests are performed to measure how badly affected the nerve is.
What is the Treatment?
Use painkillers to ease the pain, try and avoid over use activities of your wrists (excessive squeezing, gripping, wringing). A removable wrist splint is often advised as a first active treatment especially at night. If symptoms continue to be intrusive surgical opinion should be obtained. Decompression of nerve prevents symptoms from getting worse, existing symptoms more often than not improves but may stay the same.
Written by Kanthan Theivendran, Gautam Tawari and Marcus Bateman.



